Phimosis is a pathologic inability to retract the foreskin in uncircumcised men. Penile cancer is more common in men with Phimosis. Penile cancer though an uncommon medical condition, is highly associated with mortality and other adverse reactions. Penile cancer leads to physical genital disfigurement that may interfere with normal male voiding patterns, disable normal penetrative intercourse, lead to psychological and emotional disturbance and at times even death. The presence of the phallus associated with its potency and fertility defines the masculinity in our society. Penile cancer affects male self-esteem and may lead to depression. To know the fact that penile cancer is a largely preventable disease, where significant risk factors are modifiable could be considered either annoying if realized too late or a boon as awareness. The major risk factor that facilitates increased chances of penile cancer with greater occurrence range is the presence of Phimosis.

Precancerous conditions of the penis are changes to penis cells that make them more likely to develop into cancer. These conditions are not yet cancer. But if they are not treated, there is a chance that these abnormal changes may become cancer. Phimosis being a structural inability of a tight foreskin that cannot be retracted, when left untreated can lead to secondary complications that increase the susceptibility for penile carcinoma. The reason might be related to a number of involved conditions that results from phimosis. One such main reason is that, men with phimosis are less likely to be able to thoroughly clean the penis. Secondary manifestations of untreated Phimosis that could possibly pose to be precancerous conditions are:
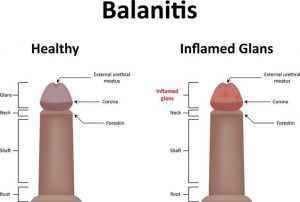
- Balanitis – when the foreskin is difficult to retract, the chances of developing infections like balanitis increase. Repeated infections are linked to a higher risk of developing some types of penile cancer as they can weaken the immune system. Recurrent inflammation of the prenuptial skin linked to penile malignancies is attributed to the presence of phimosis. Chronic inflammation is a proposed mechanism for carcinogenics in multiple types of malignancies. According to a study reported in the journal of Transitional Andrology and Urology, a history of balanitis occurred in 45% of penile cancer patients compared to 8% of controls. The report also signifies that the risk is mediated by the development of phimosis, a known risk factor for penile cancer.
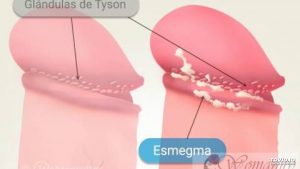
- Smegma – A number of studies have attributed an increase in penile cancer to poor penile hygiene. Sometimes secretions can build up underneath an intact foreskin. If the area under the foreskin isn’t cleaned well, these secretions build up enough to become a thick, sometimes smelly substance called smegma. Smegma is more common in men with phimosis because of the inability of the foreskin to be retracted for regular and proper cleaning of the head of the penis. Smegma is a whitish film found under the foreskin of uncircumcised males. It contains bacteria, other microorganisms, dead skin cells, mucous and other components. Evidence for a role of smegma in conditions of phimosis as the aetiology of penile cancer was obtained in an early study. The carcinogenicity of smegma associated with Phimosis was subsequently confirmed by other studies. Smegma can irritate and inflame the penis, which can increase the risk of cancer. It might also make it harder to see very early cancers.
- HPV infection – Human papillomavirus (HPV) is a widespread sexually transmitted infection. In both men and women, HPV infection can result in a spectrum of genitourinary manifestations ranging from genital warts to cancer. Penile cancer can develop following or independently of HPV infection. Basaloid and warty subtypes of penile squamous cell carcinoma are most frequently associated with HPV infection. According to a study published in The Journal of Urology Men with phimosis have increased prevalence of HPV and high-risk HPV genotypes compared with asymptomatic men. Researchers found that patients presenting with phimosis had a significantly higher rate of HPV genital infection than asymptomatic men and patients with phimosis had significantly higher prevalence of high-risk HPV. Infection with some types of HPV appears to be an important risk factor for penile cancer. In fact, HPV is found in about half of all penile cancers.
 AIDS – The majority of men who are HIV positive have been infected through the penis. Evidence demonstrates that the inner foreskin is likely to be the main portal of entry for the HIV virus in males. The large surface area of the foreskin increases the chances of acquiring HIV. The tight foreskin as in Phimosis also has greater susceptibility to traumatic epithelial disruptions (tears) during intercourse, providing a portal of entry for pathogens, including HIV. In addition, the micro environment in the preputial sac between the un retracted foreskin and the glans penis may be conducive to viral survival. Men with AIDS have a higher risk of penile cancer. This higher risk seems to be linked to their weakened immune system, which is a result of this disease. But it might also be linked to other risk factors that men with HIV are more likely to have. Circumcision to treat phimosis will help prevent HIV transmission because of keratinization of glans penis.
AIDS – The majority of men who are HIV positive have been infected through the penis. Evidence demonstrates that the inner foreskin is likely to be the main portal of entry for the HIV virus in males. The large surface area of the foreskin increases the chances of acquiring HIV. The tight foreskin as in Phimosis also has greater susceptibility to traumatic epithelial disruptions (tears) during intercourse, providing a portal of entry for pathogens, including HIV. In addition, the micro environment in the preputial sac between the un retracted foreskin and the glans penis may be conducive to viral survival. Men with AIDS have a higher risk of penile cancer. This higher risk seems to be linked to their weakened immune system, which is a result of this disease. But it might also be linked to other risk factors that men with HIV are more likely to have. Circumcision to treat phimosis will help prevent HIV transmission because of keratinization of glans penis.

Men who are circumcised cannot develop phimosis and they are not likely to accumulate smegma, develop balanitis or acquire HPV or HIV easily. Thus, men with untreated phimosis have an increased risk of penile cancer. The best known treatment for phimosis is circumcision at an early stage. Circumcision in early childhood, by eliminating phimosis, can help prevent penile cancer. Phimosis resulting from trauma or infections later in life also needs to be addressed with possible intervention of circumcision to curb the possibilities of future risk of penile cancer. Phimosis being the foremost contributing condition to the incidence of penile cancer, is associated with circumcision as the intervention for permanent solution.
Penile cancer may present as a rare neoplasm in men aged 50–70 years old. Signs and symptoms of penile cancer include sores, redness, irritation, discharge, bleeding or a lump on the penis. Fear and embarrassment in addition to social stigma result in the delay of seeking treatment by up to 1 year in 15–50% of patients. The most common site for penile cancer is the glans, which accounts for 48% of diagnoses, followed by prepuce (21%), glans and prepuce (9%), coronal sulcus (6%) and uncommonly the shaft (<2%).Phimosis is strongly associated with invasive penile carcinoma. In fact 45–85% of men with penile cancer have a history of phimosis. Phimosis causes dysplastic (pre-cancerous) changes in the skin of the preputial sac. Although length of the foreskin has been suggested as a factor, the evidence for this is weak. In a study, 52% of penile cancer cases with a long foreskin had phimosis. These findings have led to the conclusion that circumcision, as a surgical intervention to be devoid of phimosis and subsequent risk factors, may help prevent penile cancer.

